NANDA Nursing Diagnosis – A Guide to Nursing Diagnosis and Solutions
- August 15, 2024
Table of Contents
Accurate and timely nursing diagnoses are essential for providing high-quality patient care. This guide delves into the world of NANDA-I nursing diagnoses, providing a comprehensive overview of this standardized framework. By understanding the principles of nursing diagnosis and utilizing the NANDA-I taxonomy, nurses can effectively identify patient problems, develop appropriate interventions, and ultimately improve patient outcomes
What is NANDA Nursing Diagnosis?
The NANDA nursing diagnosis is a standardized framework that provides a comprehensive and structured approach to identifying and categorizing patient Nursing Diagnosis Association (NANDA), this framework is designed to enhance the account health issues within the nursing profession. Developed by the North Ameriracy and consistency of nursing diagnoses across healthcare settings. The diagnosis serves as a critical component in the nursing process, helping nurses to formulate personalized care plans that address the specific needs of their patients. By utilizing the NANDA nursing diagnosis list 2024, healthcare professionals can ensure that their interventions are both evidence-based and aligned with current best practices.
In recent years, the importance of the NANDA nursing diagnosis has grown significantly, as it offers a common language for nurses to communicate patient conditions effectively. This common language is essential for improving patient outcomes, reducing errors, and enhancing interdisciplinary collaboration. The NANDA nursing diagnosis list 2024 includes a wide range of diagnoses that cover various aspects of patient care, from physical and psychological health to social and environmental factors. By staying updated with the NANDA nursing diagnosis list 2024, nurses can provide more accurate assessments and interventions, ultimately leading to better patient care.
Statistics show that the implementation of NANDA nursing diagnosis in clinical practice has led to a measurable improvement in patient outcomes. Healthcare facilities that adopt the diagnosis framework have seen a reduction in the incidence of misdiagnosis and an increase in the efficiency of care delivery. The NANDA nursing diagnosis list 2024, which includes new and updated diagnoses, reflects the evolving nature of patient care and ensures that nurses are equipped to meet the challenges of modern healthcare.
Moreover, the diagnosis is recognized globally, making it an essential tool for nurses working in diverse healthcare environments. The widespread adoption of the NANDA nursing diagnosis list 2024 underscores its relevance in today’s healthcare landscape. As highlighted in Nursa, the diagnosis provides a critical foundation for developing nursing care plans that are both comprehensive and patient-centered. By integrating the latest trends and evidence into the NANDA nursing diagnosis list 2024, nurses can stay ahead in their practice and continue to deliver high-quality care.
For nursing professionals, staying informed about the latest updates in the NANDA nursing diagnosis list 2024 is crucial. Resources offer valuable insights and publications that help nurses keep their knowledge current. By regularly reviewing and applying the NANDA nursing diagnosis list 2024, nurses can enhance their clinical skills, contribute to better patient outcomes, and advance their careers in the ever-changing field of healthcare.
Try it - Love it - Buy it
Avail Our Free Trial Now!
What Are the Most Common NANDA Nursing Diagnoses?
Understanding the most common NANDA nursing diagnoses is essential for nurses in providing comprehensive and effective patient care. As of the NANDA nursing diagnosis list 2024, these diagnoses are critical in guiding nursing interview questions and ensuring optimal patient outcomes. Here are the seven most common NANDA nursing diagnoses you should be familiar with:
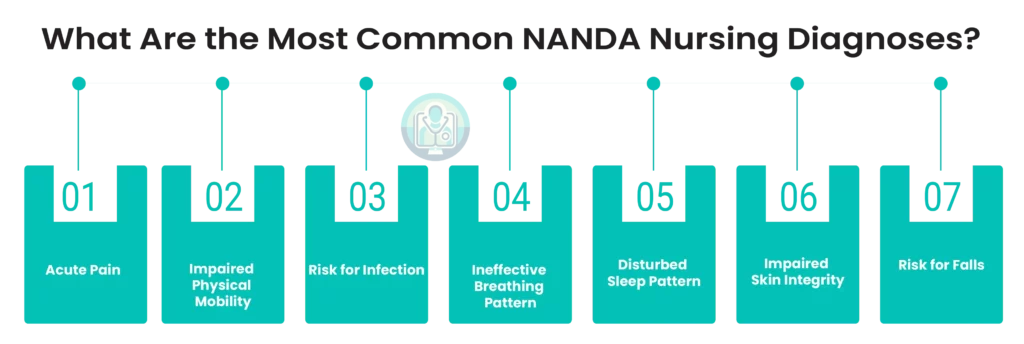
1. Acute Pain:
This diagnosis refers to an unpleasant sensory and emotional experience associated with actual or potential tissue damage. It is one of the most frequently encountered nursing diagnoses, especially in post-operative patients and those with traumatic injuries. Managing acute pain effectively is crucial for patient comfort and recovery (According to Nurselabs and IntelyCare)
2. Impaired Physical Mobility:
This diagnosis involves a limitation in independent, purposeful physical movement of the body or one of its extremities. It is particularly common in patients recovering from surgery, those with musculoskeletal injuries, or chronic conditions like arthritis. Addressing impaired mobility is vital to prevent complications such as pressure ulcers and muscle atrophy.
3. Risk for Infection:
Patients with compromised immune systems, open wounds, or those who have undergone invasive procedures are at high risk for infections. This diagnosis focuses on the vulnerability of patients to infections, which, if not managed, can lead to severe complications like sepsis.
4. Ineffective Breathing Pattern:
This diagnosis is common among patients with respiratory conditions like COPD or asthma, where the pattern of breathing is insufficient to support normal gas exchange. Timely intervention can prevent respiratory failure and improve patient outcomes.
5. Disturbed Sleep Pattern:
Often seen in hospitalized patients due to pain, anxiety, or the hospital environment, this diagnosis addresses the disruption in the quantity and quality of sleep that affects a patient’s recovery and overall well-being.
6. Impaired Skin Integrity:
This diagnosis is particularly prevalent in bedridden patients or those with chronic conditions like diabetes. It refers to a state where the skin is at risk of breakdown, potentially leading to ulcers and infections.
7. Risk for Falls:
This is a critical diagnosis for elderly patients or those with mobility impairments. It focuses on the potential for injury due to falls, which are a major concern in healthcare settings due to their impact on patient safety and recovery.
These diagnoses, as listed in the NANDA nursing diagnosis list 2024, are integral to the nursing process. They enable nurses to assess, diagnose, plan, implement, and evaluate care effectively. Staying updated with the latest NANDA classifications ensures that nursing care is evidence-based and aligned with current best practices.
What are the Benefits of NANDA Nursing Diagnoses?
The NANDA nursing diagnosis system is a critical framework for the nursing profession, providing standardized language and guidelines to ensure high-quality patient care. As the NANDA nursing diagnosis list 2024 continues to evolve, it remains an essential tool for nurses worldwide, enabling precise patient assessments and fostering improved outcomes. This article outlines the eight key benefits of utilizing diagnoses, emphasizing their role in modern healthcare and their alignment with the latest trends and developments in nursing practice.
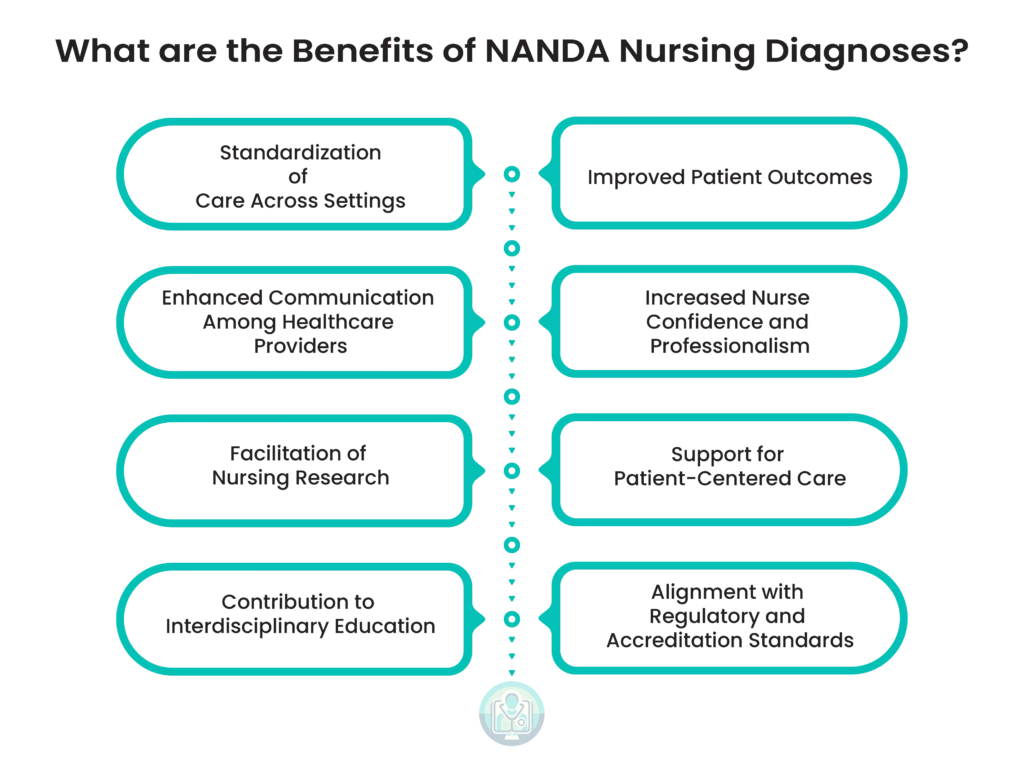
1. Standardization of Care Across Settings:
One of the primary benefits of the NANDA nursing diagnosis is its ability to standardize care across different healthcare settings. By providing a common language, the NANDA nursing diagnosis list 2024 ensures that nurses everywhere can accurately assess and document patient needs. This standardization reduces the risk of miscommunication and ensures that all healthcare providers are on the same page, which is particularly crucial in today’s increasingly complex healthcare environment.
2. Improved Patient Outcomes:
The NANDA nursing diagnosis system has been shown to improve patient outcomes by facilitating better-targeted interventions. By using a comprehensive and up-to-date NANDA nursing diagnosis list 2024, nurses can more accurately identify patient needs and implement evidence-based care plans, leading to quicker recovery times and higher patient satisfaction rates.
3. Enhanced Communication Among Healthcare Providers:
NANDA nursing diagnoses enhance communication among healthcare providers by offering a clear, standardized language. This common terminology ensures that everyone involved in a patient’s care, from nurses to physicians, understands the patient’s condition and the care plan. This is particularly important in multi-disciplinary teams, where effective communication is essential for successful outcomes.
4. Increased Nurse Confidence and Professionalism:
Using the NANDA nursing diagnosis list 2024 boosts nurse confidence and professionalism. By providing clear guidelines and a structured approach to patient care, diagnoses empower nurses to make informed decisions and take ownership of their practice. This not only enhances the quality of care but also contributes to the professional development of nurse.
5. Facilitation of Nursing Research:
NANDA nursing diagnoses play a significant role in facilitating nursing research. The standardized terminology allows for consistent data collection and analysis, enabling researchers to identify trends and develop evidence-based practices. This ongoing research contributes to the continuous improvement of the diagnosis list, ensuring it remains relevant and effective in the ever-evolving healthcare landscape.
6. Support for Patient-Centered Care:
The NANDA nursing diagnosis list 2024 supports patient-centered care by focusing on individualized patient needs. By using NANDA nursing diagnoses, nurses can develop personalized care plans that address the specific conditions and preferences of each patient, leading to more effective and compassionate care.
7- Contribution to Interdisciplinary Education:
NANDA nursing diagnoses contribute to interdisciplinary education by providing a foundation for teaching and learning in nursing programs. The standardized framework helps nursing students and professionals from other disciplines understand the nursing process, fostering collaboration and teamwork in patient care.
8- Alignment with Regulatory and Accreditation Standards:
Finally, the use of the NANDA nursing diagnosis list 2024 helps healthcare institutions meet regulatory and accreditation standards. By adhering to a recognized standard of care, institutions can demonstrate their commitment to quality and safety, which is essential for maintaining accreditation and meeting the expectations of regulatory bodies.
In conclusion, the diagnosis system offers numerous benefits, from standardizing care to improving patient outcomes. As healthcare continues to evolve, the NANDA nursing diagnosis list 2024 will remain an indispensable resource for nurses, ensuring that they can provide the highest level of care to their patients. By staying informed about the latest developments and trends, nurses can leverage these benefits to enhance their practice and contribute to the overall improvement of healthcare delivery.
NANDA Nursing Diagnosis List 2024 Table:
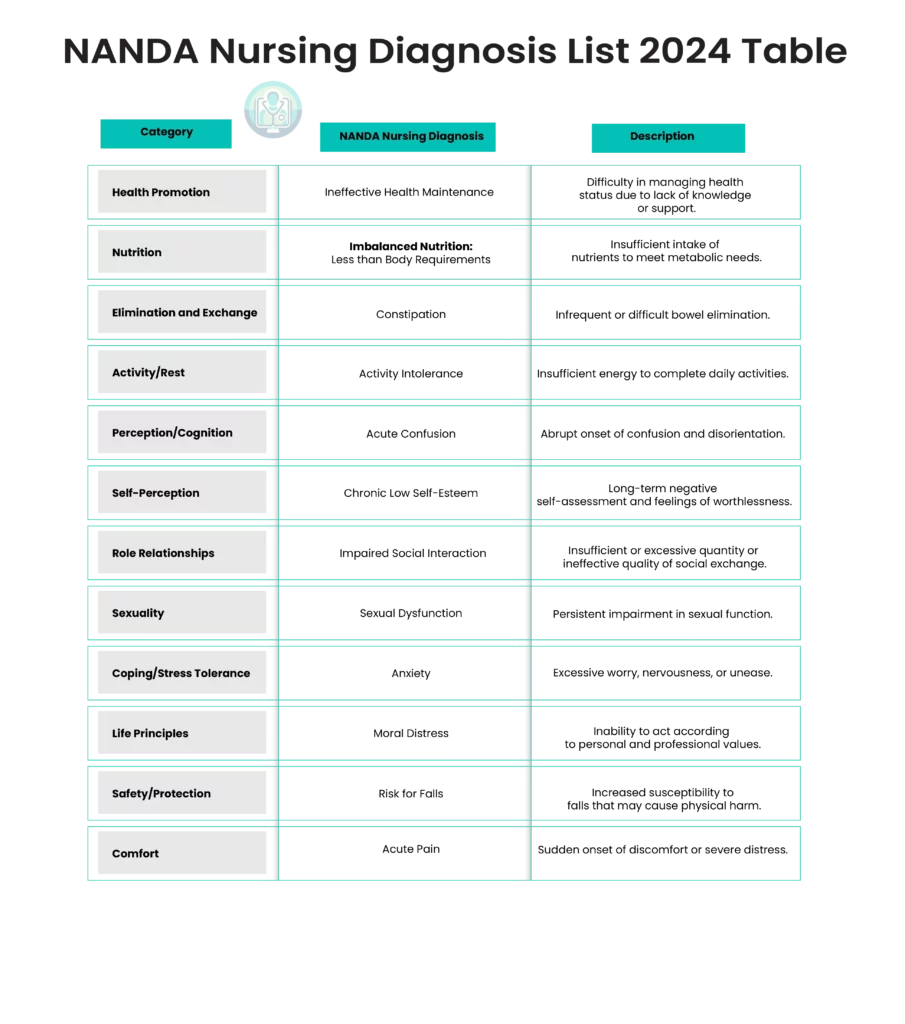
Overview of the NANDA Nursing Diagnosis List 2024:
The NANDA Nursing Diagnosis List 2024 represents a critical tool in the field of nursing, providing standardized terminology for diagnosing patient care needs. This list is widely utilized by healthcare professionals to ensure that nursing interventions are both accurate and consistent. The diagnosis framework covers a broad spectrum of patient care areas, from physical health to psychological and social well-being.
NANDA nursing diagnoses are essential for improving patient outcomes by facilitating a thorough assessment of patient needs and crafting personalized care plans. The NANDA nursing diagnosis list 2024 has evolved to reflect the latest healthcare challenges, including increased prevalence of chronic conditions, mental health issues, and the growing elderly population. According to the latest trends, the demand for nursing professionals skilled in utilizing these diagnoses is expected to grow, driven by an aging population and the expansion of healthcare services.
Incorporating technology in nursing practice is also a significant trend for 2024. The NANDA nursing diagnosis list 2024 has been updated to include new diagnoses related to telehealth and digital health management, reflecting the increasing reliance on remote patient monitoring and virtual care.
The NANDA nursing diagnosis list 2024 also emphasizes the importance of addressing nurse burnout and mental health, both for healthcare providers and patients. Nursing diagnoses such as “Anxiety” and “Chronic Low Self-Esteem” are increasingly relevant in today’s healthcare environment, where mental health is a growing concern (According to Arbor)
How to Write a NANDA Nursing Diagnosis?
Writing a NANDA nursing diagnosis is a critical skill for nurses, enabling them to make informed clinical judgments and guide patient care effectively. A NANDA nursing diagnosis involves a standardized approach that categorizes patient health issues into specific diagnoses recognized globally. The NANDA nursing diagnosis list 2024 provides an updated and comprehensive set of these diagnoses, helping nurses deliver care that is both evidence-based and patient-centered.
To write a diagnosis, a nurse must follow a systematic process that begins with a thorough patient assessment. This assessment involves gathering comprehensive data about the patient’s health status, including physical, psychological, social, and environmental factors. Based on this data, the nurse identifies the patient’s actual or potential health problems. These problems are then matched with the appropriate diagnoses from the NANDA nursing diagnosis list 2024, ensuring that the diagnosis is accurate and relevant to the patient’s condition.
The structure of a diagnosis typically includes three components: the problem (diagnostic label), the etiology (related factors), and the symptoms (defining characteristics). For example, a diagnosis might read “Impaired Mobility related to decreased muscle strength as evidenced by difficulty walking.” Here, “Impaired Mobility” is the problem, “decreased muscle strength” is the etiology, and “difficulty walking” is the symptom.
The 2024 edition of the NANDA nursing diagnosis list has been significantly revised, with over 50 new diagnoses added and several others updated to reflect current clinical practices and research. This continuous updating process ensures that the diagnoses remain relevant and useful in the ever-evolving healthcare landscape. For example, the taxonomy structure in this edition has been refined to enhance the clarity and usability of the diagnoses, making it easier for nurses to select the most appropriate diagnosis for their patients.
Moreover, the NANDA nursing diagnosis list 2024 emphasizes the importance of using these diagnoses as a tool not only for improving patient care but also for enhancing communication among healthcare professionals. By standardizing the language and criteria for nursing diagnoses, NANDA-I facilitates better interdisciplinary collaboration, ultimately leading to more cohesive and effective care plans.
Incorporating NANDA nursing diagnoses into clinical practice also aligns with the latest nursing trends for 2024, which highlight the growing emphasis on evidence-based practice, patient safety, and the integration of technology in healthcare. As nursing continues to evolve, the use of standardized diagnoses like those in the NANDA nursing diagnosis list 2024 will be crucial in ensuring that care remains consistent, high-quality, and patient-focused.
Subscribe to our Newsletter!
Subscribe our Newsletter to stay updated
How does Smart History AI integrate with NANDA Nursing Diagnosis?
Writing a NANDA nursing diagnosis is an essential skill for nursing professionals, aimed at identifying and addressing patient needs through standardized terminology. A NANDA nursing diagnosis is a critical component of the nursing process, ensuring that care is both evidence-based and patient-centered. In 2024, the updated NANDA nursing diagnosis list 2024 continues to provide a comprehensive guide for nurses to develop accurate and relevant diagnoses.
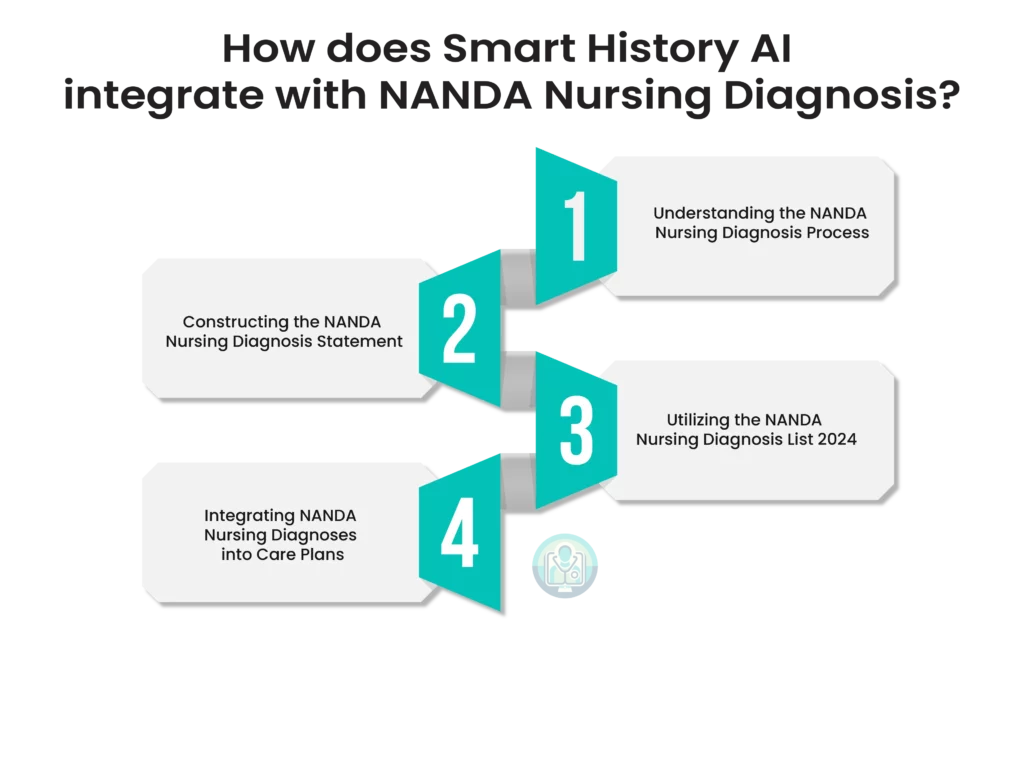
Understanding the NANDA Nursing Diagnosis Process:
The first step in writing a NANDA nursing diagnosis involves a thorough assessment of the patient’s condition. This process includes gathering data through patient interviews, physical examinations, and reviewing medical history. The NANDA nursing diagnosis list 2024 provides a structured approach to identifying health issues by categorizing them under various domains such as physical, psychological, and environmental factors.
Once the data is collected, the nurse analyzes it to identify patterns or abnormalities that indicate potential or actual health problems. The NANDA nursing diagnosis list 2024 is used to match these findings with the appropriate diagnosis. This step ensures that the diagnosis is based on standardized terminology, which enhances communication among healthcare professionals and improves patient outcomes.
Constructing the NANDA Nursing Diagnosis Statement:
A NANDA nursing diagnosis statement typically follows a specific format: Problem (P), Etiology (E), and Symptoms (S). This format is often referred to as the PES structure. The problem is identified using the NANDA nursing diagnosis list 2024, the etiology is the cause of the problem, and the symptoms are the evidence supporting the diagnosis.
For example, if a patient is experiencing shortness of breath, the nurse would use the NANDA nursing diagnosis list 2024 to find the appropriate diagnosis, such as “Impaired Gas Exchange.” The etiology might be “related to chronic obstructive pulmonary disease (COPD),” and the symptoms could be “evidenced by oxygen saturation levels below 90%.” This structured approach ensures clarity and precision in the diagnosis, which is critical for effective care planning.
Utilizing the NANDA Nursing Diagnosis List 2024:
The NANDA nursing diagnosis list 2024 is a crucial tool for nursing professionals, as it includes updated diagnoses that reflect the latest research and clinical practices. This list is regularly revised to include new diagnoses that address emerging health issues and to refine existing ones based on current evidence. For instance, the 2024 update may include new diagnoses related to mental health or chronic conditions that have gained prominence in recent years.
Using the NANDA nursing diagnosis list 2024 ensures that the nursing diagnoses are relevant and reflect the current state of healthcare. It also helps in standardizing the language used in nursing care plans, which is essential for consistency in patient care across different settings. This standardization is particularly important in large healthcare facilities where multiple nurses may be involved in a patient’s care.
Integrating NANDA Nursing Diagnoses into Care Plans:
After writing the NANDA nursing diagnosis, the next step is to incorporate it into the patient’s care plan. The care plan outlines the interventions that will be implemented to address the diagnosis and achieve the desired outcomes. The NANDA nursing diagnosis list 2024 provides a foundation for developing these care plans, ensuring that they are comprehensive and tailored to the patient’s specific needs.
The NANDA nursing diagnosis is not a static document but evolves as the patient’s condition changes. Regular reassessment and updates to the diagnosis and care plan are necessary to ensure that the patient receives the most appropriate care. The NANDA nursing diagnosis list 2024 aids in this process by offering a flexible and dynamic framework that can adapt to the changing healthcare environment.
In conclusion, writing a NANDA nursing diagnosis requires a systematic approach that begins with a thorough patient assessment, followed by the use of the NANDA nursing diagnosis list 2024 to identify and document health problems accurately. This process is integral to the development of effective care plans that improve patient outcomes and ensure high standards of nursing care. By staying updated with the latest NANDA nursing diagnosis list 2024, nurses can continue to provide relevant and evidence-based care in a rapidly evolving healthcare landscape.
Read More Blogs
See what’s trending in the medical world with our blogs